
Hyperparathyroid UK
Action4Change
It's NOT All About the Calcium Levels...
Hyper
Para
thyroid
UK
Action 4
Change

The Truth about PHPT
Established 02.09.2014
Common Questions
and
Answers:
Scroll down to read; Common Questions and Answers, kidney stones survey results, feedback about negative scans, broken bones and fractures.
Coming soon; Q&As about our tried and tested (by thousands) pre and post op mineral supplement recommendations.
Q. My doctor said my calcium is only just above range so it is unlikely the cause of my symptoms. Is he right?
A. The level of calcium does not determine the severity of symptoms, so no, your doctor is not right that a slightly elevated calcium cannot be causing symptoms. We have seen hundreds of cases where people with normocalcemic primary hyperparathyroidism who are also very symptomatic as well as people with calcium elevated just above the normal range. Their symptoms have been alleviated following successful surgery.
Q. My endocrinologist said because I am over 50 I will not benefit from surgery. I can not face the rest of my life suffering this way.
A. Age should not be a barrier to surgery. Your endocrinologist is wrong. Parathyroidectomy is curative in 95% of cases of Primary Hyperparathyroidism irrespective of age. Please see the link on our Home Page. We can provide many case stories of people in their 50s, 60s, and 70s, who have benefited greatly from parathyroid surgery. One of our members had surgery in Oxford in February 2021 aged 86 and another of our members had surgery in London aged 81. We have a lady aged 80 having surgery in Chelmsford in July 2021.
See the following comments from members over 50 who have benefitted from surgery:
HL aged 61: symptoms relieved: hot flushes, bone pain, nausea/sickness. I feel alive again and my appetite is back!
RC aged 72: symptoms relieved: Brain fog, depression, anger, itchy skin. Hair and teeth improvement. After my surgery, I felt incredible. I could have danced all night! 2 adenomas removed from the right side, and inside the thymus that had been growing 20 years.
JJB aged 55: Pain is almost completely gone, my memory and concentration have improved significantly, and almost best of all: I can sleep through the night without having to get up to pee every couple of hours. I'm wide awake all day long. Symptoms 8 years, severe osteoporosis. Stage 3 kidney failure, Doctors blamed just getting old!
BJJ aged 72 Fatigue, Gerd, itchy skin, scalp, and ear psoriasis, frequent thirst & urination Osteoporosis, pain resolved.
We asked one hundred people in a quick survey in 2016, their age at the time of surgery:
Below 50 x 14
50-55 x 33
56-60 x 22
61-65 x 12
66-70 x 16
71-75 x 03
Many people diagnosed over 50 may well have had symptoms for decades before diagnosis.
We asked 85 people over fifty how many years they had suffered from symptoms before their parathyroidectomy;
38 people suffered 1-5 years. 27 people suffered 6-10 years. 07 people suffered 11-15 years
06 people suffered 16-20 years 03 people suffered 26-30 years.
Please read Vanessa Longstaff's story on our About Us page. She was refused surgery in Scunthorpe based on being over 50. She got a second opinion from David Chadwick in Nottingham and got her life back.
Q. My endocrinologist said my calcium at 2.78 is not high enough for surgery and wants to adopt the 'watch and wait' approach. I am experiencing bone pain, memory loss, and fatigue. I am struggling to cope with my job and not sleeping at night. How long will I have to wait?
A. Primary Hyperparathyroidism is a progressive disease and may have been making you ill for some time before your calcium level was picked up. Many UK hospitals have a cut-off level of 2.85 followed by endocrinologists who will not refer for surgery. This is categorically wrong. Your endocrinologist should refer you for localising ultrasound and Sestamibi scans and refer you to an experienced parathyroid surgeon now.
Q. Can I get copies of my test results?
A. It is very important to ask for copies of every result. Get copies of your blood results and scans. So often we hear that doctors have said ' You're ok, everything is in the normal range'. It is crucial where; in the normal range your calcium, PTH, and vitamin D fall. If your calcium and PTH are both at the top of the normal range then you are NOT ok and are highly likely to have Primary Hyperparathyroidism. It is important to get several test results if your levels are not straightforward classic PHPT, to see an emerging trend remembering the non suppressive nature of a malfunctioning parathyroid gland, taking into consideration normocalcemic and normohormonal presentations of primary hyperparathyroidism. You will require calcium, PTH, Magnesium, and vitamin D tests from the same blood draw. Comparing results taken on different days is pointless.
Negative Scans
My endocrinologist won't refer me to a surgeon because my scans were negative yet my calcium and PTH are both raised and I feel this disease is ruining my life. What do I do?
Just because your adenoma was not revealed on a scan does not mean your adenoma is not there. You need to choose an experienced parathyroid surgeon. Your adenoma could be embedded in your thyroid or behind your collarbone. It is possible it did not show as a separate entity on a sestamibi scan as the thyroid also absorbs the fluid used. An experienced parathyroid surgeon will not necessarily rely on scans to find your adenoma or will request their own scans by a more experienced radiographer.
This question arises often so please do see the comments below regarding Negative Scans, and also refer to the NICE guidelines; https://www.nice.org.uk/guidance/ng132/chapter/Recommendations#referral-for-surgery ; 1.4.4 Proceed with surgery, performed by a surgeon with expertise in 4‑gland exploration, even if preoperative imaging has not identified an adenoma.
We see many cases of successful surgery following negative scans. Yes, it could indicate an ectopic gland or hyperplasia but a negative scan should never be relied upon for more than a localising guide, and should never be a reason to delay surgery. If you are told your scan is negative and it is advised to wait 'for it to grow', get a second opinion, or referral direct to an experienced surgeon.
SB: negative scans with obvious blood results should not be ignored or surgery put on hold. If a surgeon is not confident enough in his abilities to find adenomas then its reason enough to find a surgeon who will.
LS: negative scans, parathyroid adenoma behind my thyroid. 7 years, 11 fractures under Sheffield UK. Surgery in Nottingham with David Chadwick.
HB: I had 2 adenomas removed, 1 behind thyroid, and 1 in the thymus. Took thyroid nodule too. I lived in Cirencester then and went to Banbury for op - satellite hospital of Oxford Churchill. High PTH, Calcium, had very low vitamin D at diagnosis which was low/normal at the time of op with high urine calcium. Diagnosed symptomatically & by blood history from GP around 6 years; brain fog, thirst, bone pain, mood/behaviour, high blood pressure, gallstones, lethargy, bowel problems, insomnia. Post-op: bone pain immediately disappeared, blood levels, urine & BP all normal within 3 months.
JT: Parathyroid adenoma 3 cm x 1.2 cm x .5 cm Left superior, Cromwell Hospital, F Palazzo. High calcium + very high PTH. Symptoms 20+ years: fatigue, heart palpitations, hair loss, breathlessness. Paid privately - referral from GP. 6 weeks post op - most symptoms have gone. Disappeared! Scar minimal. Fatigue wearing off slowly. Recovering old self. Vit d v low. Calcium + PTH both high normal.
TE: My adenoma was found behind my thyroid. I travelled to Vancouver Canada for surgery. Symptoms 4 years for sure. High labs, poor quality life, muscle pain. Two days after surgery sight better, no joint pain.
CJ: confirmed diagnosis 2016. Adjusted calcium of 2.79 and PTH of 9. All scans negative so Endo checked for secondary then wanted to wait and see if levels went higher as “my symptoms could not be caused by my calcium levels.” Made a private appt with a surgeon who confirmed diagnosis of PHPT from my bloods and symptoms and asked me to request Endo to refer to him for surgery. Endo initially would only refer for second opinion. I have had a second negative sestamibi scan and an ultrasound in 2016 was also negative but confirmed I have a goitre and thyroid nodules. I have a date for surgery in Liverpool with Robert Hardy October 2018.
GB: all my scans were negative yet I had two adenomas removed. One was hiding behind a thyroid nodule. A good surgeon knows they are there from your blood tests.
JL: My scans found nothing but I had my op anyway. I had two glands removed one huge and another not so big. But it meant surgeon had to look at all 4 glands which in my opinion was a plus.
SSM: A negative scan can be a good thing because it means the parathyroids are right where they should be...hiding on the back of the thyroid.
MF: All my 3 scans were negative but was scheduled for an exploratory op, which was successful with Mr. Harron in Northern Ireland.
BL: My scans pre-op were negative. The operation found 3 healthy ones but didn't locate the adenoma. But the surgeon knew it was there somewhere because of my blood results. Different scans were tried and in the end, it showed up on a sestamibi.
FL: Had negative scans and my op was exploratory to find all four glands and the surgeon removed two. I am very pleased my surgeon had a good look at all four scans and do feel it’s a bit of a plus.
PEH: My scans were all negative my endo said my surgeon wouldn't contemplate surgery with my levels. He was wrong.
IZH: My adenoma didn't show on any scans but the surgeon didn't care and found it easily.
JW: I had a negative scan in April 2017, when I had the op in Oct 2017 I had two glands removed with adenomas, one gland was ok and they couldn’t find the other.
JM: I had a negative scan and had 2 adenomas removed that did not show up on any scans - so they are still there even if they do not show up on scans - had my operation on 05/04/2018
RC: Kathleen my wife also had a negative scan but three taken out by her surgeon in Sheffield.
MG: My surgeon saw something but wasn’t sure if it was the adenoma. He did the surgery, because my blood levels and urine tests clearly showed PHPT. He just checked the parathyroid glands he could see during the surgery. The spot that did show something on the scan turned out not to be the adenoma, which only goes to show that sestamibi scans aren’t the way to tell where the adenoma(s) is/are located.
NM: No tests picked mine up. They went in blind and pulled a nice big one out of my chest through the neck.
HS: Three negative scans, The surgeon removed 3 1/2 glands. Scans were a waste of time and caused the surgery to be delayed by over a year.
LM: The scan should be just another help to surgery but if negative, not a reason to stop surgery. Top surgeons don't worry, they go in and look. I had 3 negative scans so far but raised PTH and elevated calcium pointed to primary hyperparathyroidism. David Chadwick found and removed my 6 mm adenoma.
JR: parathyroid adenoma in thymus and another in the tracheal esophageal groove. I live in Lincoln. Lincoln surgeon referred on to Royal Hallamshire in Sheffield where I had surgery. First symptoms 27 years ago. I didn't have negative scans but they all showed different results, so they were all negative for something.
Deva Boone from NPC. 30 May 2016 during a live Q&A in our group: The sestamibi scan will light up the thyroid and the parathyroid tumour. If the parathyroid tumour is right next to the thyroid (which would be the most common place for it), then the scan may be "negative" because the tumour is right next to the thyroid, which is larger and lit up. When we get a pre-op sestamibi scan on someone who has never had a parathyroid operation, we don't care at all about a negative scan - it just means the parathyroid tumor is next to the thyroid, where it should be.
Kidney Stones and Primary hyperparathyroidism.
Please note: An updated NICE guideline on renal and ureteric stones was published on 9 January 2019. See link below.
Many of our members had kidney stones a long time before PHPT was diagnosed. Doctors need to check your calcium to rule out PHPT as a cause for your kidney stones early on.
Hyperparathyroid UK Action 4 Change became stakeholders on the NICE Renal and ureteric stones: assessment and management guidelines, in the hope of PHPT was flagged as a necessary test to either confirm or rule out as a cause.
https://www.nice.org.uk/guidance/NG118
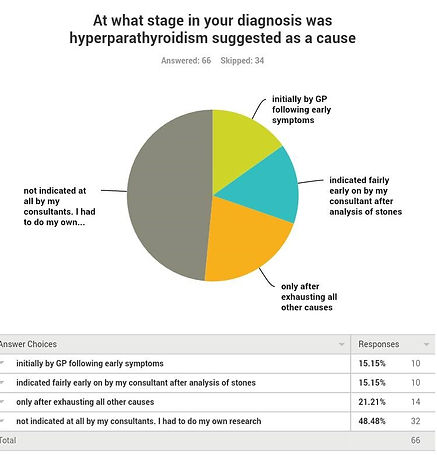
This question is asking which symptoms lead to a diagnosis of kidney stones.
The largest segment /percentage had symptoms but they did not lead their doctors to a diagnosis of kidney stones.
Many patients had to do their own research into their symptoms and realised their symptoms were kidney stones as a result of primary hyperparathyroidism. Our survey result of how many years people suffered kidney stones before find out the cause is not only sad but quite sickening. We hope the new NICE guidelines due December 18 followed by NICE guidelines for PHPT will stop this occurrence and lead to a more timely and efficient diagnosis.


The results speak for themselves and strongly suggest the need for analysing stones and testing for primary hyperparathyroidism
Once again these results speak for themselves and strongly suggest the need to test for primary hyperparathyroidism as a cause for kidney stones and the importance of early treatment (parathyroidectomy).

